Practice point

Decision-making around gastrostomy tube feeding in children with neurologic impairment: Engaging effectively with families
Posted: May 11, 2018 | Reaffirmed: Jan 11, 2024
Principal author(s)
Sanjay Mahant, Eyal Cohen, Katherine E Nelson, Peter Rosenbaum; Canadian Paediatric Society, Hospital Paediatrics Section
Paediatr Child Health 2018, 23(3):209–213 
Abstract
Children with neurologic impairment may not be able to feed safely or sufficiently by mouth to maintain an adequate nutritional state. Gastrostomy tube (G-tube) feeding is an important, often essential, intervention in such situations. However, many parents and families struggle with the decision to proceed with G-tube feeding. This practice point reviews common reasons for decisional conflict in parents and explores key aspects of life with G-tube feeding. A framework for shared decision-making and the International Classification of Functioning, Disability and Health (ICF) approach are highlighted. Practical recommendations for clinicians on engaging with families for decision-making around this life-changing intervention are provided.
Keywords: G-tube; ICF; Shared decision-making
To supplement or provide total nutrition to children with a severe neurologic impairment, gastrostomy tube (G-tube) insertion can be an important medical intervention when oral feeding is unsafe, inadequate or inefficient. While no randomized controlled trials of G-tube feeding have been conducted, evidence from systematic reviews of observational studies shows that G-tube feeding can improve nutritional status, as measured by weight [1]. Prospective studies have associated G-tube use with other benefits: reduced need for hospitalization and antibiotics for chest infections, decreased feeding times, decreased caregiver worry about nutrition, ease of medication administration and improvement in caregiver quality of life [1]–[4]. The impact of G-tubes on child quality of life and survival remains uncertain [1][4]. Issues such as G-tube insertion techniques, devices and complications were detailed in a 2011 article in this journal and are summarized in Table 1 [5].
One systematic review (which included Canadian studies) showed that decisions about G-tube feeding can be challenging for both families and clinicians, for three main reasons [6]. First, quality evidence for the efficacy of G-tube feeding—especially non-nutritional outcomes—is lacking. Clinicians might, for example, point to feeding studies on aspiration risks as absolutely indicating the need for a G-tube when, for the child who is neither undernourished nor experiencing significant respiratory illnesses, there is little evidence to support this approach [1]. Also, substitute decision-makers often make major life decisions for non-verbal, cognitively impaired children who cannot express their own wishes or communicate their quality of life. Further, G-tube feeding can be a lifelong, life-changing intervention, which a family may feel is ‘unnatural’ because it precludes the experience of eating by mouth.
Clinical practice guidelines on nutrition support for neurologically impaired children emphasize the need to consider and respect parents’ wishes around the decision to insert a G-tube [7]. This practice point reviews the evidence and conceptual frameworks and provides practical recommendations to help support families struggling with this decision. Gastrojejunal (GJ)-tube and jejunostomy (J-tube) feeding are not discussed specifically.
WHAT IS DECISIONAL CONFLICT, AND WHY DO FAMILIES EXPERIENCE THIS WHEN CONSIDERING G-TUBE FEEDING?
Decisional conflict can occur when trying to choose one course among competing options. Conflict is more likely to occur when the choice involves risk, uncertainty about outcome, feelings of loss or regret, or when a choice compromises or challenges personal values [8]. One systematic review of G-tube feeding found that parents of children with a neurologic disability often experience decisional conflict around this intervention [6]. Three broad sources of decisional conflict are identified in Figure 1 [6][9]:
- Context: The unique circumstances of each child and family
- Values: A struggle between the value and meaning (for parents) of oral feeding and potential losses associated with G-tube feeding
- Processes of care: Inadequate information-sharing and support for families
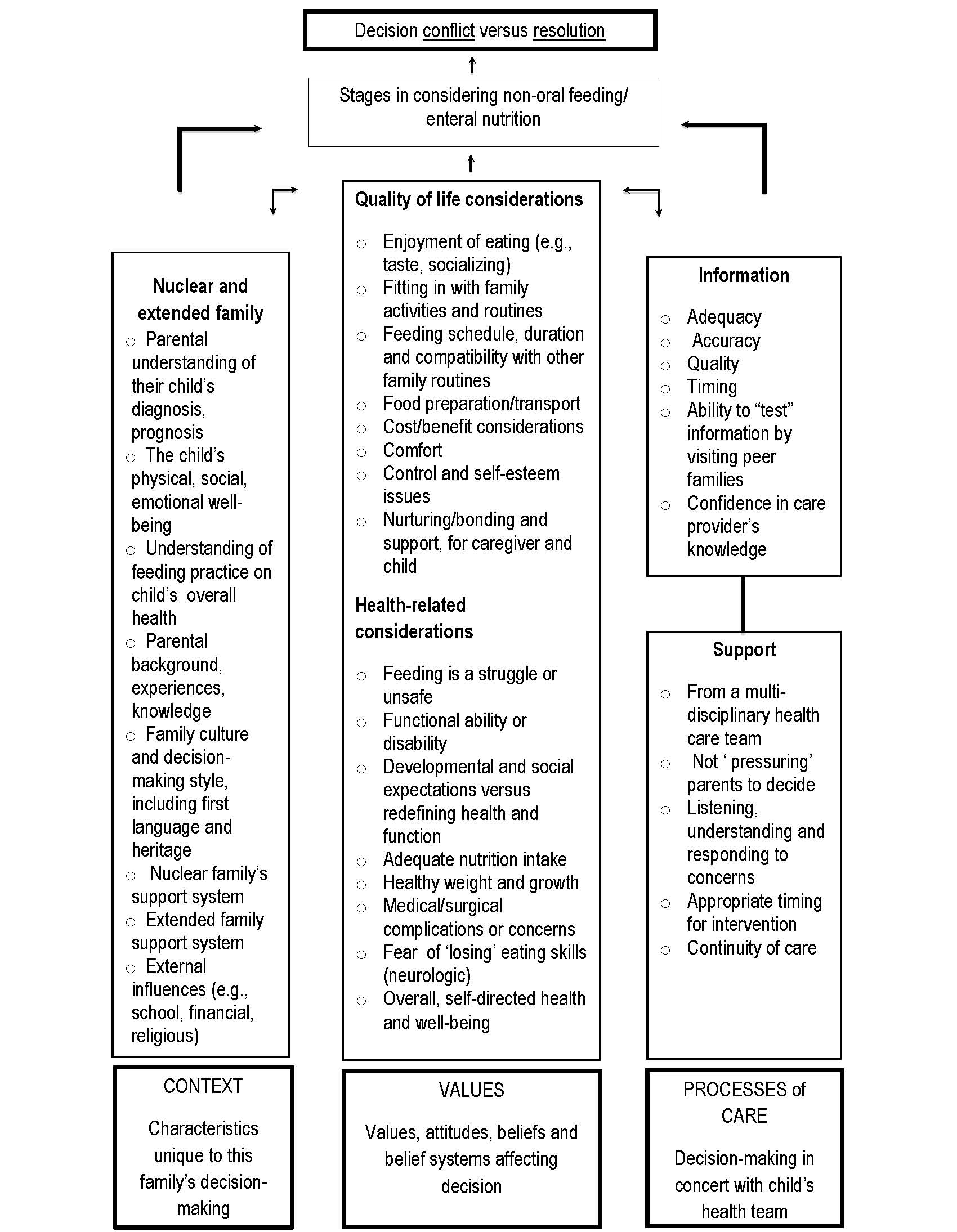 |
| Figure 1. Decisional conflict and resolution in parental decision-making around G-tube feeding [from references (6) and (9)]. |
The special value or meaning that parents attach to feeding by mouth—enjoying food and eating, the social experience, mealtimes as opportunities for nurturing and bonding—versus the ‘disability’ that their child’s G-tube may represent—are central to this struggle. For many parents, the time spent feeding their child by mouth is an expression of love, a time for close contact that is also a ‘typical’ parent-child interaction and a source of intrinsic satisfaction. The choice between oral and G-tube feeding is a trade-off between the symbolic meanings of feeding by mouth and the practical task of delivering adequate nutrition.
The clinician and parent may disagree regarding the value placed on the enjoyment of feeding by mouth versus its risks (e.g., potential for aspiration). This potential for disagreement can also contribute to parents’ decisional conflict.
WHAT CAN WE LEARN FROM FAMILIES WITH G-TUBE-FED CHILDREN?
One systematic review examined the experiences of families following G-tube placement in children with a neurologic impairment [10]. Parents described both the positive and negative impacts of G-tube feeding on family life and on their child, including the child’s physical health and quality of life, parental caregiving and stress, family function and relationships within the family and with the health care system. They described positive benefits for the child’s weight gain and happiness, caregiver quality of life and family flexibility. There were also challenges: feeding and respiratory complications for the child, increased care needs, new family stresses and the burden of more trips to seek medical care. Family and child experiences varied greatly among studies.
THE INTERNATIONAL CLASSIFICATION OF FUNCTIONING, DISABILITY AND HEALTH (ICF)
The ICF is a classification system developed by the WHO to code the components of health [11]. The framework looks beyond disease to focus on each individual’s capacity for function, activity and participation within their own environment and personal context. The ICF’s broader perspective on health also helps clinicians to guide conversations with families about decision-making.
For children with a neurologic impairment, the G-tube option could be discussed as a safety or efficiency issue (i.e., focusing on impairment) and/or as a corrective measure (i.e., focusing on undernutrition). However, the ICF’s biopsychosocial framework invites discussion of how G-tube feeding might enhance a child’s participation in family life, by decreasing long feeding times and increasing opportunities to engage in other enjoyable social activities. The ICF perspective encourages clinicians to see beyond the G-tube as a biomedical intervention and consider its impacts on child function, activity and participation.
RECOMMENDATIONS FOR CLINICIANS
Shared decision-making
Considering the pros and cons of G-tube feeding with each family will optimize decision-making. As noted above, there is often a degree of uncertainty about the ‘best’ treatment option for a given child. Uncertainty may stem from the lack of quality evidence, the child’s unique circumstances, optimal timing for this intervention or the family’s assessment of risks and benefits based on personal values. What one parent considers a prolonged feeding time may not appear that way to another. In shared decision-making, the health care professional exchanges information with families about benefits, risks and impacts of treatment options, while parents provide information and insight about personal values and preferences. Together, clinicians and caregivers determine a course of action and treatment. Remember: Each family is different in terms of how they wish to participate in decision-making, and clinician approaches need to be tailored accordingly.
Conversations and approaches
Expanding the conversation with families about G-tube feeding can engage them more constructively in the decision-making process (see Table 2) [12]. The child’s capacity to engage and share in decision-making should always be considered [13]. However, children with a neurologic impairment may also have cognitive impairment that prevents them from participating in decision-making around health in a meaningful way.
These conversations should do more than review procedure or weigh risks and benefits. They should also explore and clarify the family’s context, broad goals, values and preferences concerning G-tube versus oral feeding (Figure 1). Start by asking open-ended questions. Consider asking: “Have you any thoughts on G-tube feeding for your child?” “Do you think your child might benefit?” “What matters most about eating to you and your child?” What worries you about feeding your child?” “How can I help make this decision easier for you?” Many parents worry that their child cannot feed orally at all, so when appropriate, it is helpful to reassure them that some oral feeding (e.g., for enjoyment and stimulation) is still possible.
Be sure to include the everyday implications of G-tube feeding in discussion with families. Understanding family context (Figure 1) is key to addressing how parents view the potential impact of this intervention on their child’s daily life, on their own lives and on family life in general (Figure 2). Being familiar with context also provides opportunities to explore and allay fears and discuss adaptation strategies. It can help to explore how the child will function in different settings. Consider asking: “How will this child be supported at school?” “How will the family be supported at home?” “Do the parents know that the child can join them at meal times to share the social experience of eating together?” “Will there be extra costs and how will these be managed?” Families often benefit from the involvement of extended family (e.g., grandparents) or other caregivers in decision-making. Being sensitive to the language being used with families can help to frame G-tube feeding in positive terms.
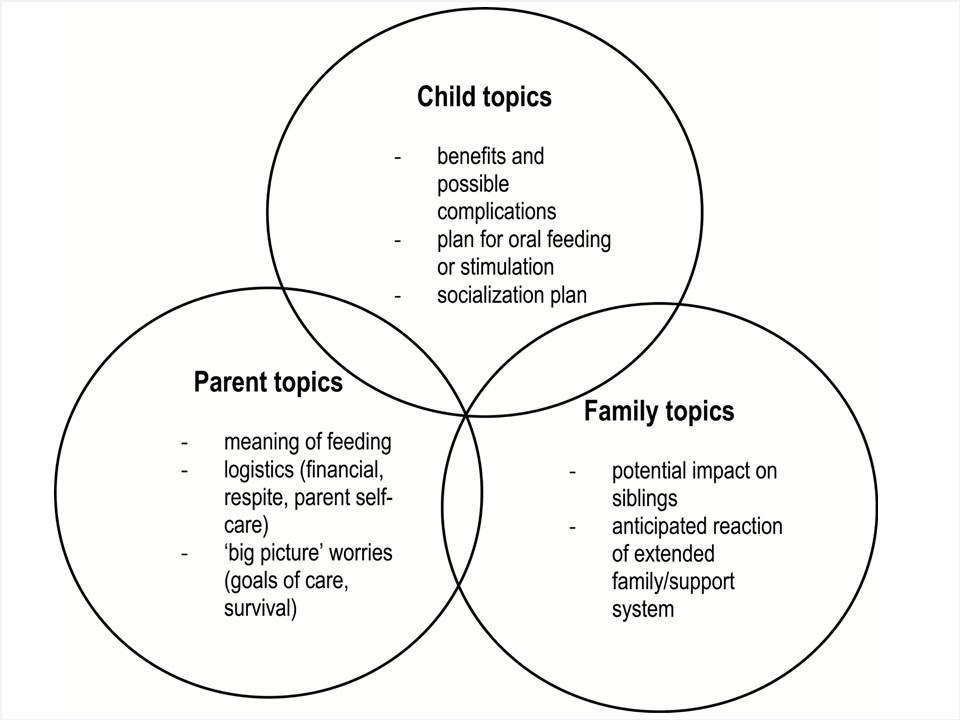 |
| Figure 2. G-tube issues to explore with families. Adapted from reference [10]. |
Opting for G-tube insertion is almost never the result of an emergency, so it is helpful to take extra time for decision-making. However, some families will want to intervene quickly, while others favour not intervening at all. For some families, nasogastric tube feeding may be an acceptable interim intervention until they can consider the options fully. Information may need to be repeated and issues discussed on several occasions as parents digest information, do their own research and think over the decision. Families should feel free to raise concerns and not feel pressured by the health care team. Education sessions and printed or web-based information from a local health centre can help parents learn about techniques of placement and the care and management of longer-term issues. Some parents will wish to meet other families with G-tube feeding experience to gain perspective and learn how they manage in everyday life.
Acknowledgements
This practice point was reviewed by the Nutrition and Gastroenterology, Community Paediatrics and Bioethics Committees of the Canadian Paediatric Society, as well as by the CPS Developmental Paediatrics Section.
CPS HOSPITAL PAEDIATRICS SECTION
Executive members: Eyal Cohen MD (past President), Marie-Joëlle Doré-Bergeron MD (President-Elect), Jessica Foulds MD (member at large), Gilbert Lam MD (Resident liaison), Gemma Vomiero MD (member at large), Jennifer Walton MD (President), Kevin Weingarten MD (Secretary-treasurer)
Principal authors: Sanjay Mahant MD, Eyal Cohen MD, Katherine E. Nelson MD, Peter Rosenbaum MD
CPS HOSPITAL PAEDIATRICS SECTION EXECUTIVE (2023-24)
Members: Melanie Buba MD FRCPC (President), Sepideh Taheri MD (President-Elect), Sidd Thakore MD (Past President), Geert 't Jong MD PHD (Secretary-Treasurer), Peter Gill FRCPC MD PHD MSC (Member at Large), Jennifer Lee Wiebe MD (Member at Large)
References
- Ferluga ED, Sathe NA, Krishnaswami S, Mcpheeters ML. Surgical intervention for feeding and nutrition difficulties in cerebral palsy: A systematic review. Dev Med Child Neurol 2014;56(1):31–43.
- Sullivan PB, Juszczak E, Bachlet AM, et al. Gastrostomy tube feeding in children with cerebral palsy: A prospective, longitudinal study. Dev Med Child Neurol 2005;47(2):77–85.
- Sullivan PB, Juszczak E, Bachlet AM, et al. Impact of gastrostomy tube feeding on the quality of life of carers of children with cerebral palsy. Dev Med Child Neurol 2004;46(12):796–800.
- Mahant S, Friedman JN, Connolly B, Goia C, Macarthur C. Tube feeding and quality of life in children with severe neurological impairment. Arch Dis Child 2009;94(9):668–73.
- Soscia J, Friedman JN. A guide to the management of common gastrostomy and gastrojejunostomy tube problems. Paediatr Child Health 2011;16(5):281–7.
- Mahant S, Jovcevska V, Cohen E. Decision-making around gastrostomy-feeding in children with neurologic disabilities. Pediatrics 2011;127(6):e1471–81.
- Marchand V, Motil KJ; NASPGHAN Committee on Nutrition. Nutrition support for neurologically impaired children: A clinical report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr 2006;43(1):123–35.
- Légaré F, O’Connor AM, Graham ID, Wells GA, Tremblay S. Impact of the Ottawa Decision Support Framework on the agreement and the difference between patients’ and physicians’ decisional conflict. Med Decis Making 2006;26(4):373–90.
- Adams RC, Elias ER; Council On Children With Disabilities. Nonoral feeding for children and youth with developmental or acquired disabilities. Pediatrics 2014;134(6):e1745–62.
- Nelson KE, Lacombe-Duncan A, Cohen E, et al. Family experiences with feeding tubes in neurologic impairment: A systematic review. Pediatrics 2015;136(1):e140–51.
- WHO. International Classification of Functioning, Disability, and Health: Children and Youth Version ICF-CY. Geneva, Switzerland: WHO, 2007. apps.who.int/iris/bitstream/10665/43737/1/9789241547321_eng.pdf (Accessed August 17, 2017).
- Mahant S, Cohen E, Rosenbaum P. Decision-making about assistive technology interventions in children with disabilities: Considerations for service providers working with families. Keeping Current, CanChild Centre for Childhood Disability Research. www.canchild.ca/en/resources/34-decision-making-about-assistive-technology-interventions-in-children-with-disabilities-considerations-for-service-providers-working-with-families. (Accessed August 17, 2017).
- O’Connor AM, Bennett CL, Stacey D. Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews 2017;4:CD001431.
Disclaimer: The recommendations in this position statement do not indicate an exclusive course of treatment or procedure to be followed. Variations, taking into account individual circumstances, may be appropriate. Internet addresses are current at time of publication.
Last updated: Feb 8, 2024

