Position statement
Child and youth injury prevention: A public health approach
Posted: Nov 2, 2012 | Reaffirmed: Jan 1, 2020
Principal author(s)
Natalie L Yanchar, Lynne J Warda, Pamela Fuselli; Canadian Paediatric Society, Injury Prevention Committee
Abridged version: Paediatr Child Health 17(9): 511
Abstract
The majority of child and youth injuries are preventable. This statement provides background, direction and a statement of commitment to the issue of child and youth injury prevention in Canada. It acts as a foundation to build upon by focusing first on definitions, scope and priorities for injury prevention. It also describes the burden and patterns of unintentional injury, and the principles of effective intervention for prevention. A list of resources for obtaining data and evidence-based information is included. This statement can also be used for broad-based injury prevention advocacy.
Key Words: Canada; Children; Injury; Prevention; Public health; Youth
Defining injury
Injury is defined as “the physical damage that results when a human body is subjected to energy that exceeds the threshold of physiological tolerance or results in lack of one or more vital elements, such as oxygen”.[1] The terms intentional and unintentional denote whether or not an injury was meant to harm the victim.[2] Intentional injuries include suicide and self-harm, homicide, assault and child abuse or neglect. This position statement will focus on unintentional injuries.
The global burden
In 1990, 10% of the 51 million deaths worldwide were due to injury.[3] It is projected that by 2020, this figure will increase to 8.4 million annually, making injury the greatest single cause of loss of healthy years of human life, especially among children and young adults.[4][5] According to the WHO’s 2008 World Report on Child Injury Prevention, approximately 950,000 children aged 17 and under were killed by an injury in 2004, and 87% of these were due to unintentional and potentially preventable causes.[1] Injury has been described as the “neglected disease of modern society”, [6] an “invisible epidemic”, and “the principal public health problem in (North) America today”.[7]
Because injuries remain the leading cause of child and youth death and disability, prevention must be incorporated into child health strategies. According to the WHO, if high income countries were to implement programs using proven-effective interventions which considered the special vulnerability of children, more than a thousand children’s lives would be saved each day.[1] Some countries began implementing strong injury prevention (IP) policies and infrastructure several decades ago, and now achieve the lowest injury rates in the world. A commonly cited example is Sweden. If Canada enjoyed the same child injury rate as Sweden, from 1991 to 1995:[1]
- 1233 children would not have died.
- 23,000 to 50,000 would not have been hospitalized.
- More than 250,000 would not have visited emergency departments.
Robust data and research are needed to develop effective IP interventions. Yet, many low- and middle-income countries lack the surveillance systems necessary for identifying priority areas and high-risk groups, while others with robust systems lack data specific enough to inform effective interventions.[1]
The burden of injury in Canada
In Canada, injury is the leading cause of death for not only children, but for all Canadians between the ages of one and 44. It ranks fourth among causes of death for all ages and is the leading cause of potential years of life lost (PYLL) before the age of 70.[8][9] Unintentional injuries, specifically, are the leading cause of PYLL in Canada and a major cause of hospitalization.[10][11] Aboriginal people, people living in rural settings, children and youth, and especially young men, are particularly vulnerable to injury.
Consider some striking injury facts:
- Between 1994 and 2003, approximately 390 Canadian children age 14 years and under died from unintentional injuries annually, while another 25,500 were hospitalized.[9]
- In 2004, injuries to Canadians cost $19.8 billion in health care costs and lost productivity, of which $16.0 billion resulted from unintentional causes. Of this, almost $3 billion could be accounted for by falls and transport-related injuries to children and youth from birth to 19 years of age.[11]
Causes of child and youth injury in Canada vary by age due to many factors, including child development and exposure to hazards. The three leading causes of injury-related deaths are motor vehicle collisions (MVCs) (17%), drowning (15%) and threats to breathing (11%) (Table 1).[12] Falls are the leading cause of hospitalization (37%), with all other causes of injuries accounting for less than 10% of hospitalizations (Table 2). [13]
|
TABLE 1: |
||||
|
Under 1 year |
1 to 4 years |
5 to 9 years |
10 to 14 years |
15 to 19 years |
|
Threat to breathing (54%) |
Motor vehicle traffic crash (22%) |
Motor vehicle traffic crash (58%) |
Motor vehicle traffic crash (55%) |
Motor vehicle traffic crash (71%) |
|
Motor vehicle traffic crash (18%) |
Drowning (21%) |
Drowning, Fall, Fire/Flame (6% each) |
Drowning (13%) |
Poisoning (7%) |
|
Drowning (15%) |
Threat to breathing (19%) |
Threat to breathing (5%) |
Fall (7%) |
Drowning (6%) |
|
TABLE 2: |
||||
|
Under 1 year |
1 to 4 years |
5 to 9 years |
10 to 14 years |
15 to 19 years |
|
Fall (46%) |
Fall (39%) |
Fall (56%) |
Fall (39%) |
Fall (24%) |
|
Threat to breathing, Fire/Hot object/substance (6% each) |
Poisoning (15%) |
Struck by/against an obstacle, Pedal cyclist non-traffic (7% each) |
Struck by/against an obstacle (15%) |
Motor vehicle traffic crash (21%) |
|
Poisoning (5%) |
Fire/Hot object/substance (7%) |
Motor vehicle traffic crash (7%) |
Motor vehicle traffic crash, Pedal cyclist non-traffic (8% each) |
Struck by/against an obstacle (14%) |
General concepts of injury epidemiology and injury prevention
The “Injury pyramid”
The injury pyramid (Figure 1) refers to the incidence and severity rate of injuries by referring to a general relationship between injury deaths, admissions to hospital and visits to the emergency department. The exact ratio between deaths, admissions and visits varies depending on the mechanism of injury and population studied. However, in general terms, for every fatally injured victim, there are many more who sustain serious but nonfatal injuries.[14]
The Haddon matrix
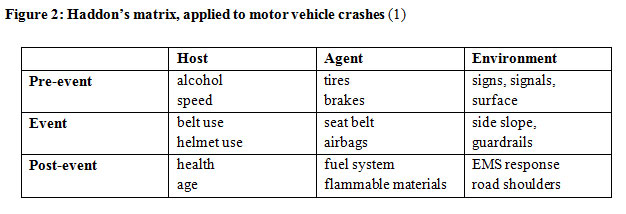
In 1949, John Gordon demonstrated that injuries are the result of harmful interactions between the host, the disease vector and the environment.[15] William Haddon later proposed examining these entities at each of three temporal phases of an injury: pre-event, the injury event itself and post-event. He produced a “phase-factor” matrix of nine cells for which various strategies to prevent or control injuries could be developed (Figure 2).[16]
The need for prevention
The frequency, severity and potential for life-long disability and death, as well as the significant economic costs involved, make injury a leading health problem and major public heath issue in Canada. With rising health care costs and the understanding that many injury cases fare poorly despite optimal treatment, prevention is undoubtedly the best approach to address this burden. Injury prevention, like immunization, has the potential to be among the greatest public health achievements of the 21st century. Injury-related death and disability rates have declined significantly over the past several years, a trend which can be attributed to the effectiveness of IP interventions, reduced exposure to risks, better trauma care or a combination thereof. Between 1994 and 2003, the overall death rate for childhood injury in Canada dropped by 37% and the hospitalization rate by 34%.[9] More specifically, over this same period, motor vehicle occupant death and hospitalization rates in children 0 to 14 years of age declined by 46%.[9] Better engineering, car seat legislation and enforcement, and social marketing are widely credited with increasing rates of seat belt and car seat use, saving thousands of lives.[17] Yet despite these and other measures, injuries remain the number one cause of death in Canadians under the age of 45.[8]
MVCs are the leading cause of injury-related deaths in Canada: an estimated 68 children age 14 years and under are killed and another 880 seriously injured each year.[17] The leading causal factors for serious and fatal collisions are still driving speed, impaired driving and lack of occupant restraint. These variables are also current priority areas for road safety and a number of evidence-based initiatives address the marketing and sale of alcohol, impaired driving legislation and enforcement, speed reduction campaigns and enforcing occupant restraint legislation. [18]
Regrettably, some proven prevention strategies remain underutilized. When used correctly, car seats reduce the risk of death by 71% for infants and by 54% for children one to four years of age, and reduce the risk of hospitalization in children age four and under by 67%.[19][20] Booster seats provide 59% more protection for young children than seat belts alone.[21] Yet it is estimated that anywhere from 44% to 81% of car seats are not used correctly and that nearly three-quarters of Canadian children four to nine years of age are not transported in booster seats.[22]-[25] A recent analysis of child passengers sustaining severe MVC-related injuries revealed that 92% of infants, 74% of toddlers and 96% of school-aged children were not restrained appropriately at the time of the crash.[26] Compounding the problem of misuse is that not all provinces and territories have mandated car and booster seat use for infants and young children, and harmonization of best practices is lacking.[27] It is imperative that all Canadian provinces and territories implement best practice legislation to protect these vulnerable road users.
Another proven-effective injury prevention strategy inconsistently implemented in Canada is helmet use for cycling. The human skull can be shattered by an impact of only 7 to 10 km/h, yet young cyclists typically ride at speeds averaging 11 to 16 km/h.[28][29] Traumatic brain injuries are the leading cause of severe injury to children on bicycles, accounting for 29% of all cycling-related hospital admissions.[9] A properly fitted helmet protects the head by absorbing the force from a crash or fall, decreasing the risk of traumatic brain injury by as much as 88%.[30][31] Up to four out of five brain injuries could be prevented if every cyclist wore a helmet.
Promoting helmet use for cyclists is vital. Across Canada, head injury rates among child and youth cyclists are about 25% lower in jurisdictions with helmet legislation compared to those without.[32] Yet helmet wearing is still not the norm across Canada, particularly for older children and adults. A 2002 survey by Safe Kids Canada showed that only 45% of children 11 to 14 years of age wore bike helmets.[33] All provinces and territories must enact comprehensive bicycle helmet legislation for all ages because adult role modelling increases compliance by children and youth.[32]
The Canadian Paediatric Society has published a number of evidence-informed position statements on other IP policies, such as mandating playground standards, enforcing helmet use for skiing and snowboarding, and restricting children and youth from operating ATVs and snowmobiles. Provinces and territories need to enact harmonized policies and legislation to concur with best practice recommendations.
A population health framework for injury control
A population health framework acknowledges that a variety of factors, impacting at different levels (individual, family, community), influence health. Such factors include social status, income, physical environment, biology and genetic endowment, personal health practices, behaviour, culture and social environment. Such variables must be considered when developing and evaluating IP strategies.
Gender
Among Canadian children aged 14 and under, the proportion of unintentional injury deaths and hospitalization by gender is 63% male and 37% female.[13] The evidence indicates that boys experience more injuries than girls from about two years of age on. Some theories about gender differences in injury relate to potential differences in predisposition, such as higher impulsivity and activity levels in boys. Other theories look at socialization. Parents tend to treat boys differently when it comes to reacting to risk-taking in play—boys get more encouragement to take risks, while girls get more words of caution.[34] Boys engage in more risk-taking than girls and appraise risk differently.[34] Boys are also more likely than girls to attribute injuries to bad luck rather than their own behavioural choices, meaning that an injury is less likely to deter repeating the risky behaviour.[34] Among young children (toddlers, preschoolers), boys require more supervision than girls and are more resistant than girls to being redirected away from a risk-taking activity they want to pursue.[34]
Aboriginal children and youth
Injury is the leading cause of death in Aboriginal children and youth. Twenty-six percent of all deaths among First Nations people are caused by injuries, compared with six percent in the general Canadian population.[35] Almost one in five First Nations children younger than 12 years of age included in the 2002/03 Regional Longitudinal Health Survey had experienced at least one injury serious enough to seek medical attention within the previous year, compared with 10% of peers in the general population.[36] In youths 12 to 17 years of age, 49.5% of First Nations youth reported injuries requiring treatment, which is more than twice the national rate.[36] First Nations disability rates are reported at 31%, double the national rate, with a large proportion attributed to injuries.[37] A recent CPS statement on injuries in this population underlines their higher, multi-factorial exposure to risks relating to living in remote areas, the distance required to access medical assessment and treatment, housing characteristics, alcohol and substance abuse, and poverty. While some injury prevention interventions have been designed and evaluated in some First Nations communities, modifications must be considered for implementation elsewhere and for applying other types of strategies.[38][39]
Rural versus urban settings
Canadian agricultural workers face more hazards in the workplace than their counterparts in many other occupations. An average of 12 children younger than 10 years of age are killed annually and 110 are hospitalized due to injuries sustained on farms.[40] Boys in agricultural settings are three to four times more likely than girls to sustain a serious injury.[40] Younger children are brought onto the work site to be supervised, while older children are often engaged in farm work. Many children and youth also use off-road vehicles such as all-terrain vehicles (ATVs) for work, transportation and recreation in rural and remote areas; [27] some are using farm equipment at a very young age. While age- and development-related guidelines for children’s agricultural tasks are available and have been evaluated, their dissemination and uptake in Canada are limited.[41][42]
Socio-economic status
The relationship between socio-economic status and health outcomes is a consistent theme in the epidemiological literature, including that related to injury. The growing evidence that higher social and economic status is associated with better health has led most researchers to conclude that these factors are fundamental determinants of health.[43] Socioeconomic gradients have been associated with risks of falls, burns, motor vehicle injuries, poisonings, as well as with intentional injuries such as assault and homicide. However, research is lacking on effective interventions to reduce the risks associated with these gaps.[44][45]
Principles of injury prevention
Researchers estimate that over 90% of unintentional injuries could be prevented. Certainly, more comprehensive injury research is needed. Yet if current IP strategies were fully implemented, it is estimated that the burden of injury could be reduced by as much as 40%. Strategies that include combining efforts—education, engineering/environment changes and enforcement/legislation—are the most successful.[46]
The E’s of injury prevention
As injury prevention theory dictates, a multi-tiered public health approach that concurrently and comprehensively targets Education, Enforcement/legislation and Engineering offers the most effective strategy for prevention.[14] Interventions must include both active and passive elements. Education refers to increasing public awareness of high-risk injuries as well as best practices to encourage voluntary adoption of safer behaviours. Enforcement refers to establishing and enforcing safety regulations, legislation and public policy which promote reduction of injury risks (eg, highway traffic laws). Engineering refers to designing safer products and environments (eg, vehicles, roads).[14] Active measures require conscious action by individuals to prevent or minimize the risk of injury, such as using a safety belt or booster seat. Passive measures do not require an individual to act to prevent injury, and are often more effective in situations where active measures are less reliable and inconsistently applied. Passive measures include airbags and external impact protection in automobiles, smoke alarms in homes, sprinkler systems in buildings and industry regulations that ensure safer products.[14]
Injury prevention surveillance and research
In many countries, leadership and coordination along with sustained infrastructure support have resulted in significant gains in combatting injury.[8] In 2001, UNICEF ranked Canada 18th out of 26 Organisation for Economic Co-operation and Development (OECD) nations with regard to child injury rates. The Canadian rate is approximately double that of top-ranked Sweden.[37]
Effective injury prevention and control require a comprehensive and integrated surveillance system that can effectively monitor injuries and collect essential data on the circumstances of injury, including: mechanisms, causes, risk factors, treatment modalities and outcomes.[37] However, current injury data collection remains fragmented in Canada and comes from a variety of sources (eg, the police, firefighters, coroner’s offices and the health care system). The inability to link various databases and the presence of gaps in key data elements have made more comprehensive surveillance a necessary basis for maximizing research opportunities and developing effective strategies to combat injury.
Research remains the cornerstone of evidence-based decision making in health. To effectively combat injury in Canada, more evidence is needed to determine burden and need, causes and risk factors, as well as the efficacy and optimal delivery of specific interventions. Research must focus on injury in the public health context, including associations and interactions with the social determinants of health.[37] However, funding for injury research is discordant with need: despite injury’s ranking as the fourth-largest disease process with respect to economic burden in Canada, research spending on injury prevention strategies ranks fifteenth.[8] Canada must invest more strategically to ensure that its most precious commodity, our children and youth, grow up healthy, safely, and to their fullest potentials.
Effective strategies to reduce injuries require comprehensive research and a variety of evidence-informed approaches to intervention.
Opportunities for action
Preventable injuries impose a heavy social and economic burden on Canadians, including health care expenses, disability, lost productivity, hospital wait-times and other costs.[11] Many proven solutions, such as education, the enforcement of bike helmet use for all ages and child passenger restraints, are extremely cost-effective yet remain underutilized. The long-term outcomes of effective strategies to combat this epidemic are invaluable.
Canada needs to invest in injury prevention with the goals of improving collaboration and coordination of efforts—from research to knowledge transfer to practice—and of strengthening linkages among federal, provincial/territorial and regional IP agencies and partners. A long-term strategy is needed that is comprehensive, sustainable and adequately resourced.[37]
While some jurisdictions have dedicated centres for IP, other provinces and territories lack this level of coordination, financial support and resource provision. Injury risks remain irrespective of jurisdiction, however, and as a health care issue, they require appropriate investment by public health at all levels of government. Included in this action should be the commitment to targeted reductions in injury rates across the full spectrum of injury causes for all Canadians. A pan-Canadian injury prevention strategy is needed, with policies that build on current foundations of IP and are guided by stakeholders and partners with expertise in this public health priority.
Recommendations
Health professionals and all levels of government must work together to reduce the burden of child and youth injury in Canada by:
- Investing in a pan-Canadian injury prevention (IP) strategy that includes leadership, policy coordination, research, surveillance, public education and social marketing.
- Supporting the development of a national IP body to help implement this strategy and to coordinate IP activities by stakeholders across the country.
- Educating the public about injury risk, and influencing behaviour change through social marketing and school-based curriculums.
- Influencing and implementing best practice, evidence-informed legislation and policies that support IP, which are harmonized across all jurisdictions and that address the social determinants of health associated with injury risk (eg, alcohol and substance abuse).
- Enforcing existing IP legislation and regulations.
- Creating safer, supervised environments for children and youth to live, learn, play and travel in.
- Sustaining and advancing current and new injury surveillance, including:
- out-patient injuries (eg, the Canadian Hospital Injury Reporting and Prevention Program, the National Ambulatory Care Reporting System),
- hospitalized trauma patients (eg, the National Trauma Registry), and
- trauma deaths (eg, a national medical examiners death database).
- Sustaining and advancing current and new IP research programs.
Health care practitioners should:
- Include injury prevention in their practices (eg, supporting car seat and home safety knowledge in prenatal classes, well-child care, hospital-based care and discharge planning).
- Advocate for local and regional IP policies and actions as outlined above.
Recommended resources
National
- Canadian Paediatric Society: www.cps.ca
- Canadian Paediatric Surveillance Program: www.cpsp.cps.ca
- Safe Kids Canada: www.safekidscanada.ca
- ThinkFirst Foundation Canada: www.thinkfirst.ca
- Safe Communities Canada: www.safecommunities.ca
- SMARTRISK: www.smartrisk.ca
- Canadian Collaborative Centres for Injury Prevention (CCCIP): www.ccip.ca
- Canadian Institute of Child Health (CICH): www.cich.ca
- Canadian Red Cross: www.redcross.ca
- Canadian Agricultural Injury Surveillance Program (CAISP): www.cor-sbac.ca
- A Journey to the Teachings, Health Canada: http://publications.gc.ca/site/eng/339983/publication.html
Provincial/territorial
- Child Safety Link: www.childsafetylink.ca
- Injury Prevention Centre: www.injurypreventioncentre.ca
- British Columbia Injury Reporting and Prevention Unit (BCIRPU): www.injuryresearch.bc.ca
- Atlantic Collaborative for Injury Prevention (ACIP): http://www.acip.ca/
- Saskatchewan Prevention Institute: www.preventioninstitute.sk.ca/
Statistics and research
- Canadian Institute for Health Information (CIHI): www.cihi.ca
- Canadian Hospitals Injury Research and Prevention Program (CHIRPP): www.phac-aspc.gc.ca/injury-bles/chirpp
- Canadian Institute for Health Research (CIHR): www.cihr-irsc.gc.ca
- Statistics Canada: www.statcan.gc.ca
- Injury Prevention Journal (IP): http://ip.bmjjournals.com
- Safety Lit: www.safetylit.org
Government websites
- Health Canada: www.hc-sc.gc.ca
- Public Health Agency of Canada (PHAC): www.phac-aspc.gc.ca
- Transport Canada: www.tc.gc.ca
International
- The World Health Organization (WHO): www.who.int/violence_injury_prevention/en/
- Safe Kids Worldwide (SKWW): www.safekids.org
- International Society for Violence and Injury Prevention (ISVIP): www.isvip.org
- EuroSafe, European Association for Injury Prevention and Safety Promotion—European Child Safety Alliance: http://childsafetyeurope.org/
Acknowledgements
This position statement has been reviewed by the Community Paediatrics, First Nations, Inuit and Métis Health, and Healthy Active Living and Sports Medicine Committees of the Canadian Paediatric Society, as well as by the CPS Action Committee for Children and Teens.
CPS INJURY PREVENTION COMMITTEE
Members: Claude Cyr MD; Brent E Hagel PhD; I Barry Pless MD; Jeffrey W Scott MD; Natalie L Yanchar MD (Chair); Mitchell Zelman MD (Board Representative)
Liaisons: Dominic Allain MD, CPS Paediatric Emergency Medicine Section; Pamela Fuselli, Safe Kids Canada; Robin Skinner, Public Health Agency of Canada
Principal authors: Natalie L Yanchar MD; Lynne J Warda MD (past Chair); Pamela Fuselli
References
- World Health Organization. World Report on child injury prevention. December 2008: www.who.int/violence_injury_prevention/child/injury/world_report/report/en/index.html (Accessed May 25, 2012).
- Christoffel KK, Scheidt PC, Agran PF, Kraus JF, McLoughlin E, Paulson JA. Standard definitions for childhood injury research: Excerpts of a conference report. Pediatrics, 1992;89(6Pt 1):1033.
- Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 1997;349(9061):1269-76.
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease. Lancet 1997;349(9064):1498-504.
- Murray CJ, Lopez AD (eds.) The Global Burden of Disease. Geneva: WHO, Harvard School of Public Health, World Bank, 1996.
- National Academy of Sciences. Accidental Death and Disability: The Neglected Disease of Modern Society. Washington DC: National Academy Press, 1996.
- National Academy of Sciences. Injury in America: A Continuing Public Health Problem. Washington, DC: National Academy Press, 1985.
- Canadian Health Services Research Foundation and Canadian Institutes of Health Research, Institute of Health Services and Policy Research, 2007. Listening for Direction: Final report to Health Canada: www.chsrf.ca/Libraries/Listening_for_Direction/LfDIII-NRFinal_ENG_05_09_08.sflb.ashx (Accessed May 25, 2012).
- Safe Kids Canada. Child & Youth Unintentional Injury: 1994-2003; 10 Years in Review. National Report 2006: www.mhp.gov.on.ca/en/prevention/injury-prevention/skc_injuries.pdf (Accessed May 25, 2012).
- Statistics Canada, Canadian Vital Statistics, Death Database, and Demography Division (population estimates). Potential years of life lost, population aged 0 to 74, by selected causes of death and sex, Canada, provinces and territories, annual: http://www.communityaccounts.ca/SALandscape/1_8_pyll.htm#RANGE!TFtn (Accessed June 6, 2012).
- Smartrisk, 2009. The Economic Burden of Injury in Canada: www.smartrisk.ca/downloads/burden/Canada2009/EBI-Eng-Final.pdf (Accessed May 25, 2012).
- Public Health Agency of Canada. Analysis of mortality data from Statistics Canada (unpublished ).
- Public Health Agency of Canada. Analysis of hospitalization data from the Canadian Institute for Health Information (unpublished).
- Razzak JA, Sasser SM, Kellermann AL. Injury prevention and other international public health initiatives. Emerg Med Clin North Am 2005;23(1):85-98.
- Gordon JE. The epidemiology of accidents. Am J Public Health 1949;39(4):504-15.
- Haddon W Jr. A logical framework for categorizing highway safety phenomena and activity. J Trauma 1972;12(3):193-207.
- Canadian Council of Motor Transport Administrators. National occupant restraint program (NORP) 2010. Accessed January 2012.
- Transport Canada. Canada’s road safety targets to 2010. Accessed January 2012.
- Kahane C. An evaluation of child passenger safety: The effectiveness and benefits of safety seats. Washington, DC: U.S. Department of Transportation. National Highway Traffic Safety Administration, 1986. Report No. 806 890: www.nhtsa.dot.gov/cars/rules/regrev/Evaluate/806890.html (Accessed May 25, 2012).
- National Highway Traffic Safety Administration. Research note: revised estimates of child restraint effectiveness. Washington, DC: U.S. Department of Transportation. National Highway Traffic Safety Administration, 1996. Report No. 96.855: www-nrd.nhtsa.dot.gov/Pubs/96855.pdf (Accessed May 25, 2012).
- Durbin DR, Elliott MR, Winston FK. Belt-positioning booster seats and reduction in risk of injury among older children in vehicle crashes. JAMA 2003;289(21):2835-40.
- Canadian Paediatric Society, Injury Prevention Committee. Transportation of infants and children in motor vehicles (Principal author Charmaine van Schaik) Paediatr Child Health 2008;13(4):313-8:. www.cps.ca/en/documents/position/car-seat-safety (Accessed September 14, 2012).
- Margolis LH, Wagenaar AC, Molnar LJ. Use and misuse of automobile child restraint devices. Am J Dis Child 1992;146(3):361-6.
- Morris SD, Arborgast KB, Durbin DR, Winston FK. Misuse of booster seats. Inj Prev 2000;6(4):28-4.
- Snowdon AW, Hussein A, Purc-Stevenson R, et al. Are we there yet? Canada’s progress towards achieving road safety vision 2010 for children travelling in vehicles. Int J Inj Contr Saf Promot 2009;16(4):231-7.
- Chouinard A, Hurley R. Towards the development of a national child restraint survey. Transport Canada. The Canadian Multidisciplinary Road Safety Conference XV. Fredericton, N.B., June 2005.
- Safe Kids Canada. Provincial and territorial car seat and booster seat legislation: www.safekidscanada.ca/Professionals/Advocacy/Documents/26794-CarSeatLaws.pdf (Accessed May 25, 2012).
- Thompson DC, Rebolledo V, Thompson RS, Kaufman A, Rivara FP. Bike speed measurements in a recreational population: Validity of self reported speed. Inj Prev 1997;3(1):43-5.
- Canadian Bike Helmet Coalition. How to Organize a Community Project. 1994.
- Thompson DC, Rivara FP, Thompson RS. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database Syst Rev 2000(2); CD001855.
- Attewell RG, Glase K, McFadden M. Bicycle helmet efficacy: A meta-analysis. Accid Anal Prev 2001;33(3):345-52.
- Macpherson AK, To TM, Macarthur C, Chipman ML, Wright JG, Parkin PC. Impact of mandatory helmet legislation on bicycle-related head injuries in children: A population-based study. Pediatrics 2002; 110(5):e60.
- Safe Kids Canada. National Bike Helmet Survey, 2002.
- Morrongiello BA, Dawber T. Mothers’ responses to sons and daughters engaging in injury-risk behaviors on a playground: Implications for sex differences in injury rates. J Exp Child Psychol 2000;76(2):89-103.
- Health Canada, First Nations, Inuit and Aboriginal Health. Keeping Safe – Injury Prevention: www.hc-sc.gc.ca/fniah-spnia/promotion/injury-bless/index-eng.php (Accessed May 25, 2012).
- First Nations Regional Longitudinal Health Survey (RHS) 2002/3. Results for Adults, Youth and Children Living in First Nations Communities. First Nations Centre, 2005: www.naho.ca
- Smartrisk, 2005. Ending Canada’s invisible epidemic: A strategy for injury prevention: www.smartrisk.ca/downloads/publications/NS-Eng.pdf (Accessed May 25, 2012).
- Health Canada, 2009. A Statistical Profile on the Health of First Nations in Canada: Health Services Utilization in Western Canada, 2000. www.hc-sc.gc.ca/fniah-spnia/pubs/aborig-autoch/2009-stats-profil-vol2/index-eng.php (Accessed May 25, 2012).
- Canadian Paediatric Society, First Nations, Inuit and Métis Health Committee, Preventing unintentional injuries in Indigenous children and youth in Canada (Principal author Anna Banerji) Paediatr Child Health 2012;17(7):393: www.cps.ca/en/documents/position/unintentional-injuries-indigenous-children-youth (Accessed September 14, 2012).
- Canadian Agricultural Injury Surveillance Program. Summary report on agricultural injuries in Canada, 1990-2000. Accessed May 25, 2012.
- Marshfield Clinic Research Foundation, North American Guidelines for Children’s Agricultural Tasks: http://www.nagcat.org/nagcat (Accessed May 28, 2012).
- Canadian Paediatric Society, Injury Prevention Committee, Preventing injuries from all-terrain vehicles (Principal author Natalie Yanchar) Paediatr Child Health 2012;17(7): www.cps.ca/en/documents/position/preventing-injury-from-atvs (Accessed September 14, 2012).
- Scott K. A lost decade: Income equality and the health of Canadians. Paper presented at the Social Determinants of Health Across the Life-Span Conference. Toronto, November 2002. Accessed May 28, 2012.
- Brownell MD, Derksen SA, Jutte DP, Roos NP, Ekuma O, Yallop L. Socio-economic inequities in children’s injury rates: Has the gradient changed over time? Can J Public Health 2010;101(Suppl 3):S28-31.
- Laflamme L, Hasselberg M, Burrows S. 20 years of research on socioeconomic inequality and children’s unintentional injuries: Understanding the cause-specific evidence at hand. Int J Pediatr 2010;2010. pii:819687. Epub 2010 Jul 25.
- Safe Kids Canada. Making it Happen Pedestrian Safety, A Guide for Communities, 2004.
Disclaimer: The recommendations in this position statement do not indicate an exclusive course of treatment or procedure to be followed. Variations, taking into account individual circumstances, may be appropriate. Internet addresses are current at time of publication.

